The Role of Gut Microbiota in Mental Health
Source: NCBI
مدت زمان تمرین این بخش: 45 دقیقه
Paragraph 1
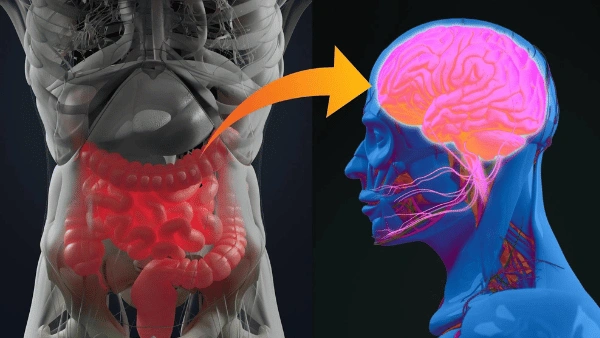
The human gut microbiota, a complex community of microorganisms residing in the gastrointestinal tract, has been increasingly recognized for its role in various aspects of health, including mental well-being. Recent research has highlighted the gut-brain axis, a bidirectional communication network that links the central nervous system with the enteric nervous system. This connection suggests that the gut microbiota can influence brain function and behavior. For instance, certain bacterial strains have been found to produce neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA), which are critical for mood regulation.
Simplified:
The human gut microbiota is a complex community of microorganisms living in the digestive tract. These microorganisms are increasingly recognized for their role in various health aspects, including mental well-being. Recent research has focused on the gut-brain axis, a communication network linking the brain with the gut’s nervous system. This connection suggests that gut bacteria can influence brain function and behavior. For example, some bacteria produce neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which help regulate mood.
Paragraph 2
A study conducted in 2020 examined the gut microbiota composition of individuals diagnosed with major depressive disorder (MDD) compared to healthy controls. The results revealed significant differences in the abundance of specific bacterial genera. Notably, individuals with MDD had lower levels of Faecalibacterium and Coprococcus, both of which are known for their anti-inflammatory properties. This finding supports the hypothesis that inflammation may play a role in the pathophysiology of depression.
Simplified:
In 2020, a study compared the gut microbiota of people with major depressive disorder (MDD) to that of healthy individuals. The study found significant differences, with MDD patients having lower levels of certain beneficial bacteria, such as Faecalibacterium and Coprococcus, which have anti-inflammatory properties. This supports the idea that inflammation may contribute to depression.
Paragraph 3
Further research has explored the potential of probiotics as a therapeutic intervention for mental health disorders. Probiotics are live microorganisms that, when administered in adequate amounts, confer a health benefit on the host. A randomized controlled trial published in 2021 investigated the effects of a multi-strain probiotic supplement on anxiety and depressive symptoms in a cohort of adults. The study found that participants who received the probiotic supplement reported a significant reduction in symptoms compared to the placebo group. These results suggest that modulating the gut microbiota could be a promising strategy for managing mental health conditions.
Simplified:
Further research has looked into using probiotics—live microorganisms that provide health benefits—as a treatment for mental health issues. A 2021 randomized controlled trial tested a probiotic supplement on adults with anxiety and depression. Participants who took the supplement reported a significant reduction in symptoms compared to those who took a placebo. This suggests that altering the gut microbiota could help manage mental health conditions.
Paragraph 4
The mechanisms by which gut microbiota influence mental health are still being elucidated. One proposed pathway involves the modulation of the hypothalamic-pituitary-adrenal (HPA) axis, which regulates the body’s stress response. Dysregulation of the HPA axis has been implicated in the development of anxiety and depression. Animal studies have shown that germ-free mice, which lack gut microbiota, exhibit exaggerated HPA axis responses to stress, further underscoring the importance of microbial presence in stress regulation.
Simplified:
The exact ways gut microbiota affect mental health are still being studied. One theory involves the hypothalamic-pituitary-adrenal (HPA) axis, which controls the body’s stress response. Disruptions in the HPA axis are linked to anxiety and depression. Studies on germ-free mice, which lack gut bacteria, show these mice have exaggerated stress responses, highlighting the importance of gut microbes in stress regulation.
Paragraph 5
Another area of interest is the role of diet in shaping the gut microbiota and, consequently, mental health. Diets high in fiber, for example, promote the growth of beneficial bacteria that produce short-chain fatty acids (SCFAs). SCFAs have been shown to have anti-inflammatory effects and to influence brain function. Conversely, diets high in saturated fats and sugars can lead to dysbiosis, an imbalance in the gut microbiota, which has been associated with increased risk of mental health disorders.
Simplified:
Diet also plays a role in shaping the gut microbiota and mental health. High-fiber diets encourage the growth of beneficial bacteria that produce short-chain fatty acids (SCFAs), which have anti-inflammatory effects and influence brain function. On the other hand, diets high in saturated fats and sugars can cause an imbalance in gut bacteria, increasing the risk of mental health disorders.
Paragraph 6
Despite the growing body of evidence linking gut microbiota to mental health, several challenges remain. One major challenge is the individual variability in gut microbiota composition, which can be influenced by factors such as genetics, diet, and environment. This variability makes it difficult to develop universal probiotic treatments. Additionally, more research is needed to understand the long-term effects of probiotic supplementation and to identify which bacterial strains are most effective for specific mental health conditions.
Simplified:
Despite the growing evidence linking gut microbiota to mental health, challenges remain. Individual differences in gut microbiota, influenced by genetics, diet, and environment, make it hard to create universal probiotic treatments. More research is needed to understand the long-term effects of probiotics and identify which bacterial strains work best for specific mental health conditions.
Paragraph 7
In conclusion, the gut microbiota represents a novel and exciting frontier in the field of mental health research. While the exact mechanisms remain to be fully understood, the potential for gut microbiota modulation to serve as a therapeutic avenue for mental health disorders is promising. Future studies should focus on elucidating these mechanisms and on developing targeted probiotic therapies that can be personalized to individual microbiota profiles.
Simplified:
In conclusion, the gut microbiota is an exciting area in mental health research. Although the exact mechanisms are not fully understood, there is potential for using gut microbiota modulation as a treatment for mental health disorders. Future studies should focus on understanding these mechanisms better and developing personalized probiotic therapies.
